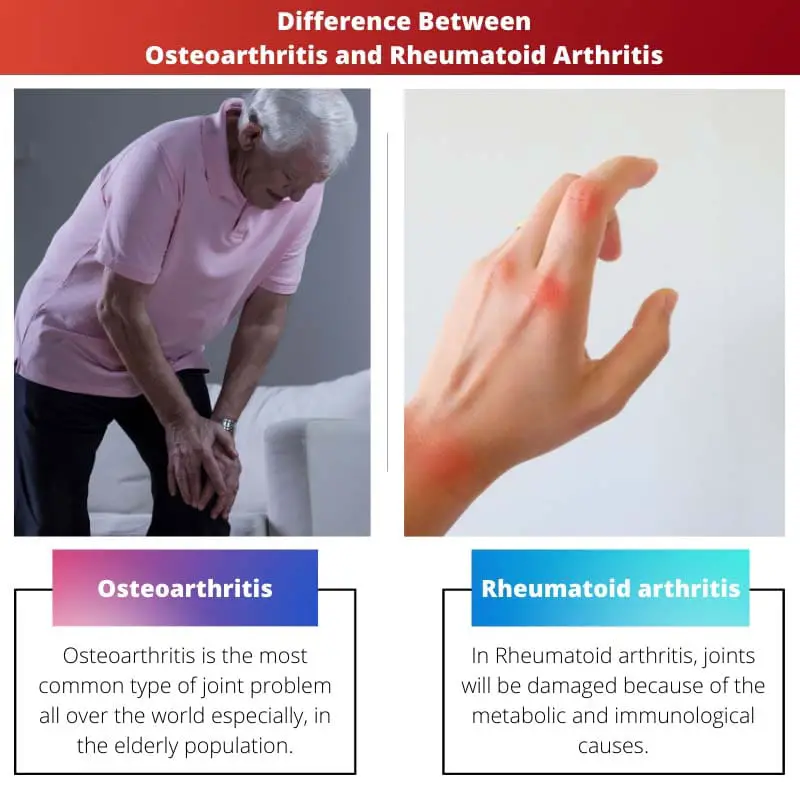
Osteoarthritis is a degenerative joint disease caused by wear and tear, primarily affecting cartilage. Rheumatoid arthritis is an autoimmune disorder leading to joint inflammation and damage. While osteoarthritis is age-related, rheumatoid arthritis can affect people of any age.
Key Takeaways
- Osteoarthritis is a degenerative joint disease caused by wear and tear, while rheumatoid arthritis is an autoimmune disorder in which the immune system attacks healthy joint tissue.
- Osteoarthritis affects cartilage, leading to joint pain and stiffness, while rheumatoid arthritis causes joint lining inflammation, resulting in pain, swelling, and deformity.
- Treatment for osteoarthritis focuses on managing pain and maintaining mobility, while rheumatoid arthritis treatment aims to reduce inflammation, manage symptoms, and slow disease progression
Osteoarthritis vs Rheumatoid Arthritis
Osteoarthritis (OA) is the most common form of arthritis. Some people call it degenerative joint disease or “wear and tear” arthritis. It occurs most frequently in the hands, hips, and knees. Rheumatoid arthritis is an autoimmune disease, which means that the immune system malfunctions and attacks the body instead of intruders.
Though these two appear like similar things, they have vast differences between them.
Comparison Table
| Feature | Osteoarthritis (OA) | Rheumatoid Arthritis (RA) |
|---|---|---|
| Type of Arthritis | Degenerative | Autoimmune |
| Cause | Wear and tear on cartilage in joints | Immune system mistakenly attacks joint lining |
| Affected Joints | Primarily weight-bearing joints (knees, hips, spine) | Can affect any joint, symmetrically (hands, feet, wrists) |
| Symptoms | Joint pain, stiffness, swelling, reduced range of motion | Joint pain, stiffness, swelling, warmth, fatigue, fever, loss of appetite |
| Onset | Usually later in life (after 40) | Can occur at any age, but most common between 40-60 |
| Progression | Gradual worsening over time | Can be episodic with flares and remissions |
| Treatment | Pain management, exercise, physical therapy, joint replacement in severe cases | Medications to suppress immune system, joint therapy, lifestyle changes |
| Disability | Can limit mobility and daily activities | Can be more debilitating and lead to joint deformities |
| Risk Factors | Age, family history, obesity, previous joint injury | Family history, smoking, obesity, environmental factors |
| Diagnosis | X-rays, MRI scans, physical examination | Blood tests, X-rays, MRI scans, physical examination |
What is Osteoarthritis?
Osteoarthritis (OA) is a degenerative joint disease characterized by the gradual breakdown of joint cartilage and underlying bone. It is the most common form of arthritis and develops with age, impacting the knees, hips, hands, and spine.
Causes and Risk Factors
- Age and Wear and Tear: OA is commonly associated with aging, as the cartilage naturally undergoes wear and tear over time.
- Joint Injury: Previous joint injuries or trauma can increase the risk of developing osteoarthritis in the affected joint.
- Obesity: Excess body weight places additional stress on weight-bearing joints, contributing to cartilage deterioration.
- Genetics: There may be a genetic predisposition to osteoarthritis, with certain genes influencing cartilage structure and function.
Pathophysiology
- Cartilage Breakdown: Gradual loss of cartilage leads to friction between bones, causing pain, swelling, and stiffness.
- Bone Changes: Over time, bone spurs (osteophytes) may form around the affected joint, further impacting joint function.
- Synovial Inflammation: The synovium, the lining of the joint, may become inflamed, exacerbating symptoms.
Clinical Presentation
- Joint Pain: Persistent pain, especially during or after movement, is a hallmark symptom.
- Stiffness: Joint stiffness, particularly upon waking or after periods of inactivity, is common.
- Reduced Range of Motion: OA can result in diminished flexibility and difficulty in performing daily activities.
- Joint Enlargement: In some cases, joints affected by osteoarthritis may appear larger due to swelling.
Diagnosis and Treatment
- Clinical Evaluation: Physical examination and imaging (X-rays, MRI) help diagnose and assess the severity of OA.
- Pain Management: Analgesics, anti-inflammatory medications, and lifestyle modifications are employed for symptom relief.
- Exercise and Physical Therapy: Strengthening exercises and physical therapy can improve joint function and alleviate pain.
- Joint Replacement Surgery: In advanced cases, joint replacement surgery may be considered to restore function and alleviate pain.

What is Rheumatoid Arthritis?
Rheumatoid arthritis (RA) is a chronic autoimmune disorder primarily targeting the joints, characterized by inflammation and joint damage. Here are detailed explanations under H4 headings:
Immune System Dysfunction
In RA, the immune system mistakenly attacks the synovium—the lining of the membranes that surround joints. This immune system dysfunction leads to inflammation in affected joints, causing pain, swelling, and potential damage to surrounding tissues.
Joint Involvement and Symptoms
RA commonly affects joints on both sides of the body, such as wrists, knees, and fingers. Morning stiffness, joint pain, and swelling are hallmark symptoms. Over time, untreated RA can result in joint deformities and limitations in mobility.
Systemic Impact
Beyond joints, RA can have systemic effects, impacting organs like the heart, lungs, and eyes. Increased risk of cardiovascular disease and other complications make early diagnosis and management crucial. Treatment involves medications to control inflammation and modulate the immune response.

Main Differences Between Osteoarthritis and Rheumatoid Arthritis
- Etiology:
- Osteoarthritis (OA): Caused by wear and tear on joints, primarily associated with aging and joint overuse.
- Rheumatoid Arthritis (RA): Autoimmune disorder where the immune system attacks the synovium, leading to joint inflammation.
- Joint Involvement:
- OA: Affects specific joints due to localized wear, commonly seen in weight-bearing joints like knees and hips.
- RA: Symmetrical joint involvement, affecting small joints in the hands and feet, but can impact any joint.
- Inflammation and Pathology:
- OA: Inflammation is secondary, primarily involving the breakdown of cartilage and formation of bone spurs.
- RA: Characterized by chronic inflammation, leading to joint swelling, pain, and potential joint damage.
- Age and Onset:
- OA: Typically associated with aging, with onset later in life.
- RA: Can occur at any age, starting between 30 and 60 years old.
- Systemic Effects:
- OA: Primarily localized to the joints, with minimal systemic impact.
- RA: Can have systemic manifestations, affecting organs like the heart, lungs, and eyes.
- Treatment Approach:
- OA: Management focuses on pain relief, lifestyle modifications, and sometimes surgical interventions like joint replacement.
- RA: Requires more aggressive treatment, including disease-modifying antirheumatic drugs (DMARDs) to suppress the immune response and reduce inflammation.